The Use of PSA Testing to Screen for Prostate Cancer in American Men
Aside from cancers of the skin, prostate cancer is the leading type of cancer for men in the United States. Prostate cancers most frequently start development in the gland cells of the prostate, known scientifically as prostate adenocarcinoma. Prostate adenocarcinoma grows characteristically slowly and is frequently an underlying cause of death for older men who die of alternative causes. Prostate cancer can be devastating because of its blind development in men who are not aware they fall victim to this disease. For this reason, prostate cancer screening has been proposed to identify cases that otherwise go unnoticed and untreated. Though these methods have been proposed, little research has been devoted to assessing the effectiveness and cost-benefit ratio for such measures.
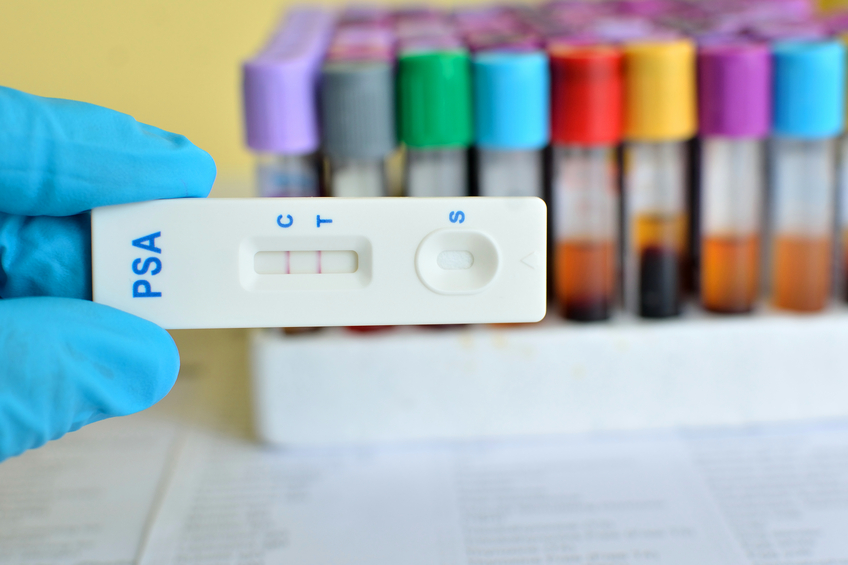
One frequently employed screening test for prostate cancer is a prostate-specific-antigen test (PSA). This screening technique hones in on the blood composition to measure the amount of PSA present. This antigen is a protein produced in the prostate gland of the bladder. Prostate cancer characteristically maintains high levels of prostate-specific-antigen in the blood and fluids, a marker for adenocarcinoma. The utilization of PSA screening began in 1988, and recommendations have fluctuated in since years. Some organizations such as the American Cancer Society propose rectal examination starting at the age of 50, while the U.S. Preventative Services Task Force rises that age to 75 based off of prevalent risk.
A recent review in the New England Journal of Medicine investigated two study groups conducting randomized clinical trials on the potential benefits of prostate cancer screening through PSA tests. Data on new cancer cases, survival rates, and stage development was investigated for all individuals in the cohort. After the follow-up period of the study terminated, more cases of prostate cancer were diagnosed in the screened group as opposed to the standard group (2820 vs. 2322). This trend persisted as the study commenced further. Most of the cases that were identified by the screening technique as well as in the standard group were at Stage II, adenocarcinoma development. The study found little difference in proportion of deaths due to prostate cancer between the screening and control group.
Risks due to screening were additionally assessed to confirm or deny its use to detect prostate cancer in a safe and efficacious manner. Few complications were observed in those individuals who were screened. More complications were observed from treatment including bleeding, infection, and trouble with urination.
Ultimately, the researchers of this report witnessed a 22% increase in diagnosis with the PSA screening test, despite some individuals marked as non-compliant (85% compliance). Researchers proposed that even more individuals may have been diagnosed if the cut off levels for prostate-specific-antigen in the blood were lower than 4 ng/mL. Due to the unobserved reduction in prostate cancer mortality from screening, age 75 was supported as the starting point for PSA screening.
Reference—
Andriole GL, Crawford ED, Grubb RL, et al. Mortality Results from a Randomized Prostate-Cancer Screening Trial. The New England journal of medicine. 2009;360(13):1310-1319. doi:10.1056/NEJMoa0810696.